Introduction:
Daratumumab-based quadruplets are the current standard of care for newly diagnosed transplant-eligible multiple myeloma (MM) patients, because of improved depth of response and survival, compared with triplet regimens without daratumumab. Since one of the primary mechanisms of action of daratumumab is the induction of antibody-dependent cellular cytotoxicity (ADCC) via the Fc-gamma receptor CD16 on natural killer (NK) cells, it is crucial to understand the role of NK cells in combination therapy. We therefore set out to comprehensively profile NK cells by flow cytometry in newly diagnosed MM (NDMM) patients treated with either daratumumab, bortezomib, thalidomide, and dexamethasone (D-VTD) or VTD.
Methods:
A subset of NDMM patients (n = 152) who were treated in the Cassiopeia trial (EudraCT: 2014-004781-15) was included in this immunomonitoring analysis. In this trial, patients were first randomized to receive either four induction cycles and two consolidation cycles of D-VTD or VTD in conjunction with autologous stem cell transplantation (ASCT). In the second part of this trial, patients who achieved partial response or better at day 100 post-ASCT were randomized to either receive daratumumab maintenance or observation for the duration of two years.
Bone marrow (BM) and peripheral blood (PB) samples were collected at study entry (baseline), and for PB at additional time points: cycle 1 day 28, cycle 4 day 28, day 100 (post-ASCT) and week 52 (maintenance). All baseline BM and PB samples and a selection of longitudinal PB samples were profiled by flow cytometry, with a focus on NK cell phenotype (CD56, CD16, CD57, DNAM-1, TIGIT, KLRG1, PD1, TIM3, NKG2A, NKG2C, NKG2D).
To identify NK cell profiles associated with minimal residual disease (MRD) negativity, baseline PB and BM data were compared between MM patients based on MRD status after consolidation. Additionally, longitudinal data of PB samples collected during treatment were assessed to understand the impact of D-VTD and VTD on NK cell profiles.
Results:
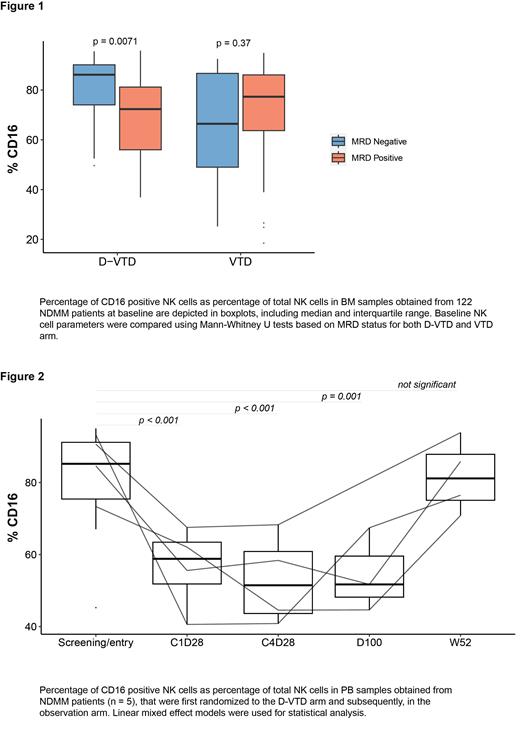
In this cohort, 49 patients out of 77 (64%) randomized to the D-VTD arm achieved MRD negativity post-consolidation, while this was the case in 28 out of 75 patients (37%) in the VTD arm (fisher exact-test, p = 0.008). Patients with a higher proportion of BM-residing NK cells expressing the ADCC receptor CD16 (median 86 vs 72%, p = 0.007), the activating receptor DNAM-1 (median 94 vs 89%, p = 0.029), or the maturation marker CD57 (median 58 vs 48 %, p = 0.049) at baseline were more likely to achieve MRD-negativity post-consolidation in the D-VTD arm (Figure 1). Notably, this association was not present in the VTD arm. Although not significant, we found a similar trend for CD16 in PB in the D-VTD arm.
During D-VTD treatment, we observed an increase in the proportion of CD56 bright and NKG2A + in PB NK-cells, and a corresponding decline in cells expressing CD16, CD57 and DNAM-1 (linear mixed effect model (LME) p <0.001). During VTD treatment we also observed a decrease in CD16 + NK-cells and an increase in CD56 bright and NKG2A + NK-cells (LME p <0.05), although these changes were more pronounced in the D-VTD arm.
In patients who were assigned D-VTD at the first randomization and were subsequently randomized to the observation arm, we observed a restoration of the proportion of CD16 +, CD57 +, and CD56 bright NK cells to baseline values at week 52 after ASCT (Figure 2). As expected, the daratumumab associated NK cell changes persisted in the group that was randomized to the daratumumab maintenance arm.
Conclusion:
This study highlights the importance of NK cell immunophenotypic profiles in bone marrow as predictive markers for MRD negativity in NDMM patients treated with D-VTD in in conjunction with ASCT. Additionally, our findings illustrate that NK cell changes associated with daratumumab return to baseline levels after treatment cessation, indicating the potential for sequential NK cell-based therapies.
In conclusion, this study not only provides valuable insights into the role of NK cells in the treatment of NDMM patients with D-VTD and ASCT, but also indicates that further research to optimize NK cell function in the context of combination therapies is warranted.
Disclosures
Moreau:GSK: Honoraria, Other: Advisory Board; janssen, celgene BMS, abbvie, sanofi, amgen, takeda, pfizer: Honoraria, Other: advisory boards. Sonneveld:Karyopharm: Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees, Research Funding; Amgen: Membership on an entity's Board of Directors or advisory committees, Research Funding. Zweegman:Celgene: Research Funding; Oncopeptides: Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding. Mutis:Takeda: Research Funding; Genmab: Research Funding; Janssen: Research Funding. Van De Donk:Janssen Pharmaceuticals, Amgen, Celgene, Novartis, Cellectis, BMS: Research Funding; Janssen, Amgen, Celgene, BMS, Takeda, Roche, Novartis, Bayer, Adaptive, Servier: Consultancy.